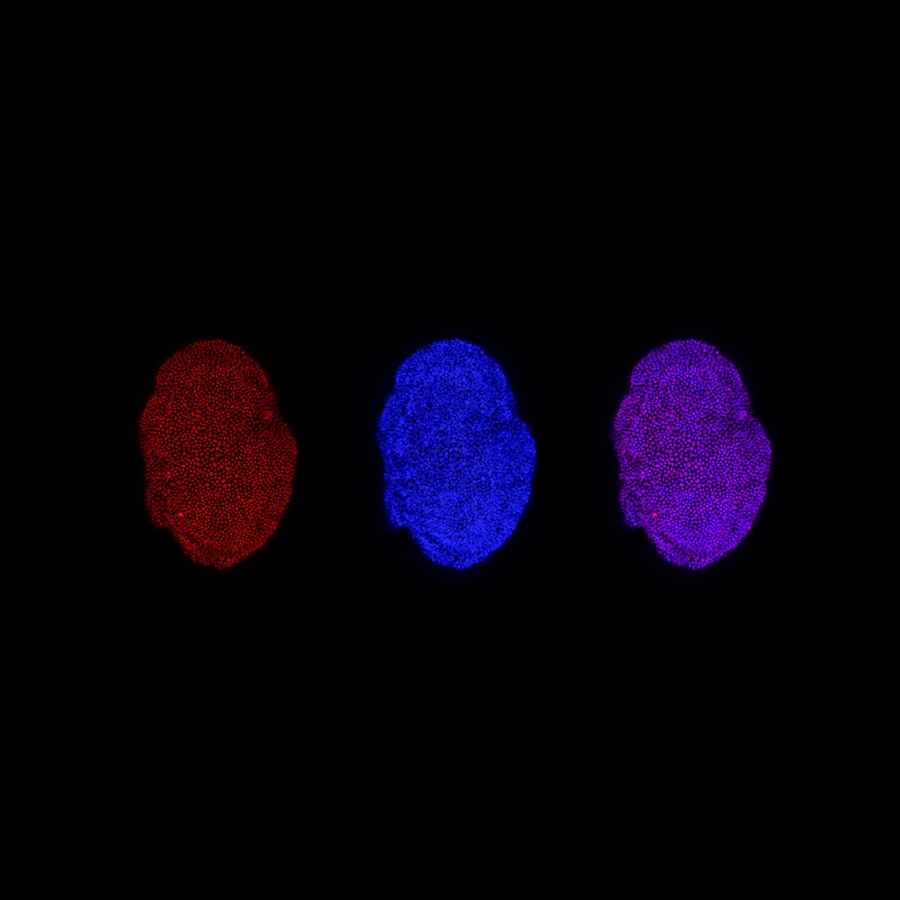
Images show a single adult liver organoid illuminated for fluroescent markers: left, to show the TET1 epigenetic mark (5-hydroxymethylcytosine) in red; centre, to show cell nuclei in blue; and right, merged to show TET1 in nuclei. From Luigi Aloia; graphic design Ludovica Bastianini.
Researchers at the University of Cambridge have uncovered a novel molecular mechanism that allows damaged adult liver cells to regenerate, paving the way for design of drugs to boost regeneration in conditions such as cirrhosis or other chronic liver diseases where regeneration is impaired. The work is described in a paper published in the journal Nature Cell Biology.
It has long been known that the human liver is one of the organs that can regenerate its own tissue after short-term injury. But chronic damage in conditions such as alcohol abuse, fatty liver disease and certain viral infections, leads to impaired regeneration and cirrhosis (scarring), with eventual loss of liver function.
The molecular mechanisms by which adult liver cells trigger the regenerative response, and how this fails in chronic liver disease, remain largely unknown. Around 30 million people across Europe suffer from chronic liver diseases, for which there is currently no cure, with liver transplants being the only treatment for liver failure. Scientists are therefore exploring how to trigger the intrinsic regenerative capacity of the liver, as an alternative means to restore function.
Researchers at the University of Cambridge’s Gurdon Institute used mouse models and liver organoids ('mini-livers' generated in the lab from mouse liver cells) to study the biological principles of adult liver regeneration. They discovered that a molecule called TET1 is produced in healthy adult liver cells during the first steps of the regenerative response, and that this process is mimicked in liver organoids, where it has a role in stimulating organoid growth.
Dr Luigi Aloia, first author of the paper and postdoctoral researcher at the Gurdon Institute, said: “We now understand how adult liver cells respond to the changes caused by tissue injury. This paves the way for exciting future work to target TET1 activity with drugs in an effort to boost cell regeneration in chronic liver disease, or in other organs where regeneration is minimal such as the brain or pancreas.”
TET1 and similar molecules are known to be essential in the developing embryo, where cells are dividing and differentiating to produce all the different organs of the body. But this study is the first to demonstrate that the activity of TET1 underpins regeneration in adult mouse liver tissue.
The adult liver is formed by two main types of cells: hepatocytes, which perform many of the liver's functions, and ductal cells, which form the network of tiny ducts delivering bile to the intestine. After acute (short-term) damage hepatocytes are able to regenerate, but after more severe injury they are not. After severe or chronic injury, the ductal cells become capable of generating both new hepatocytes and new ductal cells to replenish the liver tissue, through induction of an identity-switching process known as plasticity.
Researchers from Cambridge’s Gurdon Institute took part in the collaborative study, along with colleagues in the UK and Germany, to explore the molecular mechanism that provides ductal cells with this power to regenerate the liver tissue. They showed that a chemical switch - known as an epigenetic modification - on the ductal cell's DNA is activated by TET1. This switch allows genes to 'turn on' so that the cell can respond to changes in the environment such as damage, and activate the regeneration program when needed.
Dr Meritxell Huch, now located at the MPI-CBG, led the research and said: “Our finding pinpoints TET1 as the protein that enables plasticity of the ductal cells and their regenerative capacity in response to injury. Because the epigenetic switch activated by TET1 does not modify the genetic sequence of the cell, but the mechanism by which the genes are expressed, it represents a target that could be modified by drugs.”
Acknowledgements
The work was funded by the Wellcome Trust, Cancer Research UK and the Royal Society; Luigi Aloia holds a Horizon 2020 Marie Sklodowska-Curie Individual Fellowship.
NOTE: Since 1st October 2019 Dr Meritxell Huch has been in post as Lise Meitner Research Group Leader at the Max Planck Institute of Molecular Cell Biology and Genetics (MPI-CBG) in Dresden, Germany.
---
About the University of Cambridge
The mission of the University of Cambridge is to contribute to society through the pursuit of education, learning and research at the highest international levels of excellence. To date, 109 affiliates of the University have won the Nobel Prize./
Founded in 1209, the University comprises 31 autonomous Colleges, which admit undergraduates and provide small-group tuition, and 150 departments, faculties and institutions. Cambridge is a global university. Its 19,000-student body includes 3,700 international students from 120 countries. Cambridge researchers collaborate with colleagues worldwide, and the University has established larger-scale partnerships in Asia, Africa and America.
The University sits at the heart of the ‘Cambridge cluster’, which employs 60,000 people and has in excess of £12 billion in turnover generated annually by the 4,700 knowledge-intensive firms in and around the city. The city publishes 341 patents per 100,000 residents.
www.cam.ac.uk
About the Wellcome Trust/ Cancer Research UK Gurdon Institute
Named after its co-founder, Nobel Laureate Sir John Gurdon, the Gurdon Institute (part of the University of Cambridge) is a world-leading centre for research into the biology of development and how normal growth and maintenance go wrong in diseases such as cancer.
More than 240 scientists work in the Gurdon Institute’s purpose-built laboratories on projects ranging from breast cancer and brain development to liver regeneration and leukaemia. Many have made pioneering contributions to the fields of basic cell biology, cellular reprogramming, epigenetics and DNA repair. Institute scientists use a range of model systems such as yeast, nematode worms, fruit flies, frogs, mammalian cells and organoids to study development and disease at the level of molecules, cells and tissues.
Research conducted at the Institute has so far led to more than a dozen spin-out companies (including KuDOS Pharmaceuticals, Abcam, CellCentric, Mission Therapeutics, Gen2 Neuro and STORM Therapeutics) and five candidate drugs. One of these, the PARP inhibitor olaparib (Lynparza), has been approved worldwide for use against certain ovarian and breast cancers.
www.gurdon.cam.ac.uk
Aloia, L et al. Epigenetic remodelling licences adult cholangiocytes for organoid formation and liver regeneration (2019) Nature Cell Biology. doi: https://doi.org/10.1038/s41556-019-0402-6